Comprehensive Diabetes Management: Tools and Strategies for Better Health
Discover HealthFeed's personalized diabetes management tools, from meal planning to CGM integration, for better health.
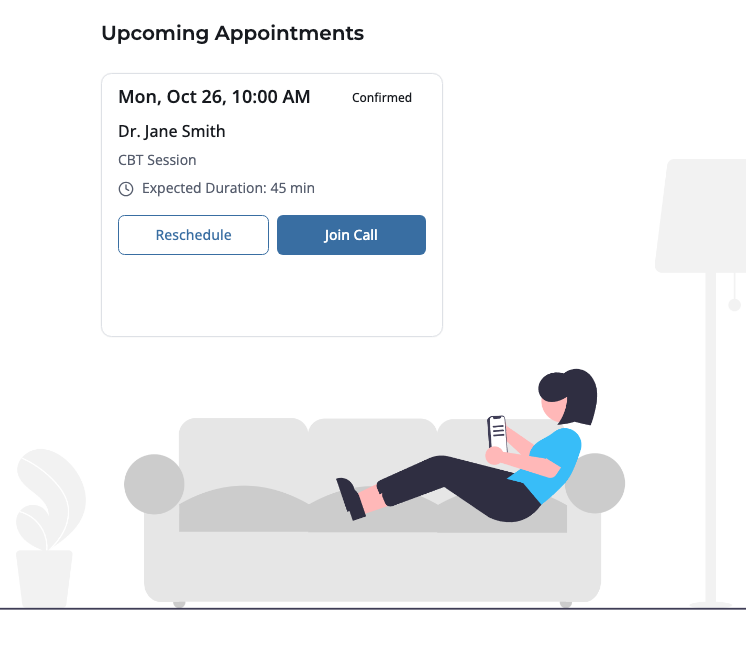
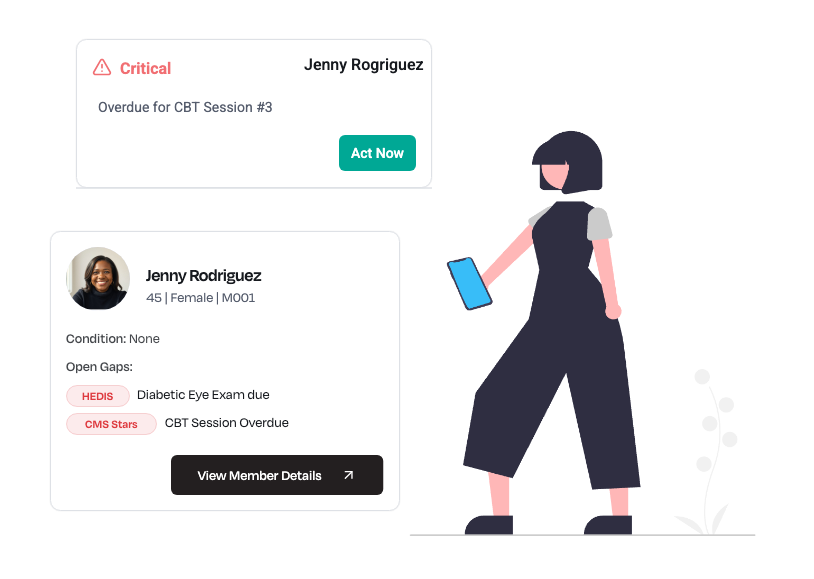
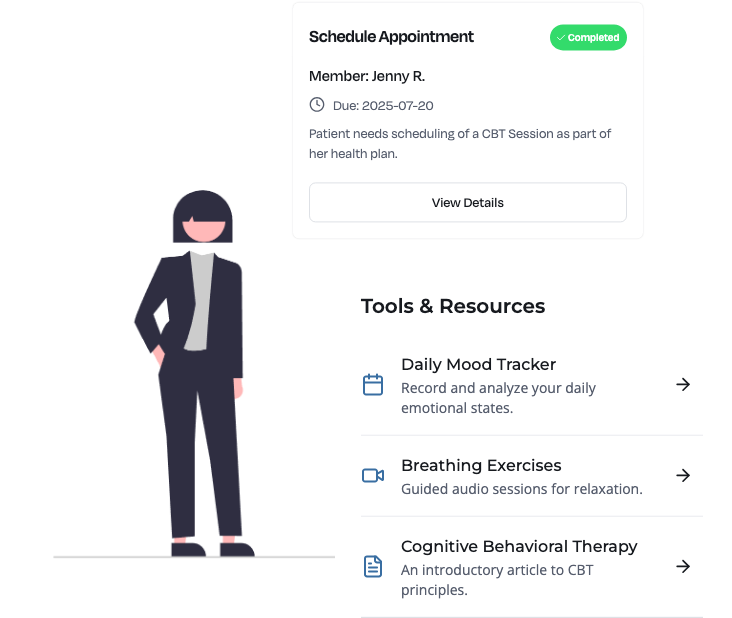
HealthFeed helps payers and providers close behavioral health gaps with personalized, multi-channel engagement, from initial screenings to long-term therapy adherence. Our platform reduces no-shows, improves follow-up rates, and streamlines care coordination across providers and support teams.


.png)
.png)
.png)




Closing care gaps isn’t just about clinical interventions. Members face everyday barriers that prevent them from accessing care and following treatment plans:
Closing care gaps isn’t just about clinical interventions. Members face everyday barriers that prevent them from accessing care and following treatment plans:
.svg)
Missed appointments delay progress and waste resources.
.svg)
Members struggle to maintain therapy and medication schedules.

.svg)
Care teams lack a unified way to reach and support members.
.svg)
Limited visibility into engagement and adherence metrics.
HealthFeed gives care teams a centralized, intelligent platform to track, manage, and engage members across their entire health journey.
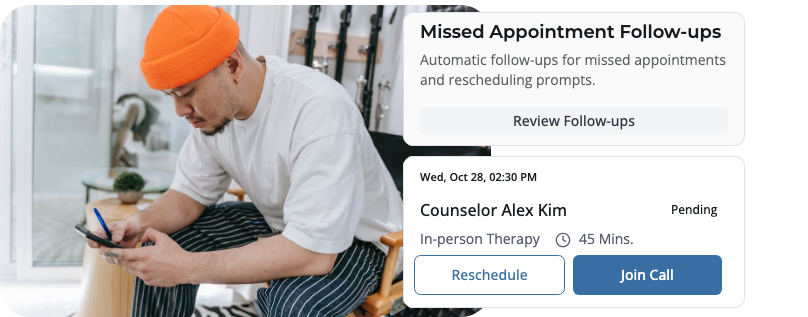
Sends reminders, confirmations, and rescheduling prompts via SMS, email, IVR, and chat.
Automates follow-ups after missed appointments to re-engage members quickly.
Tracks attendance patterns to identify high-risk no-show members for proactive outreach.
38%
reduction in no-show rates when using automated reminders delivered via SMS, email, IVR, or chat.
6%
Reduction in no show rates using automated reminders compared to no reminders.
26%
increase in program participation rates when using culturally tailored educational materials.
22%
improved therapy adherence rates when providing self-help resources in a preferred language
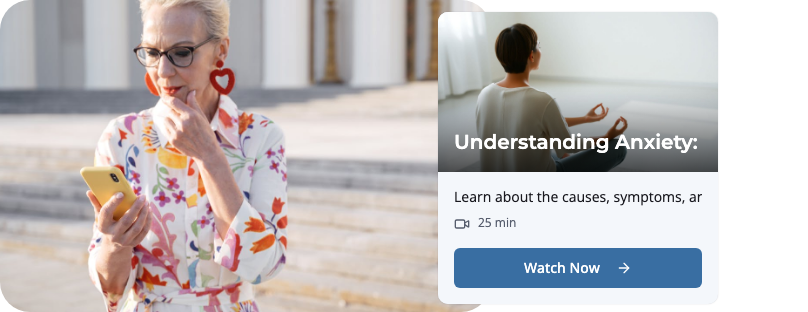
Delivers targeted content to reduce stigma and encourage participation in behavioral health programs.
Adapts materials to members’ cultural background, preferred language, and literacy level.
Provides on-demand self-help resources, including videos, articles, and coping tools.
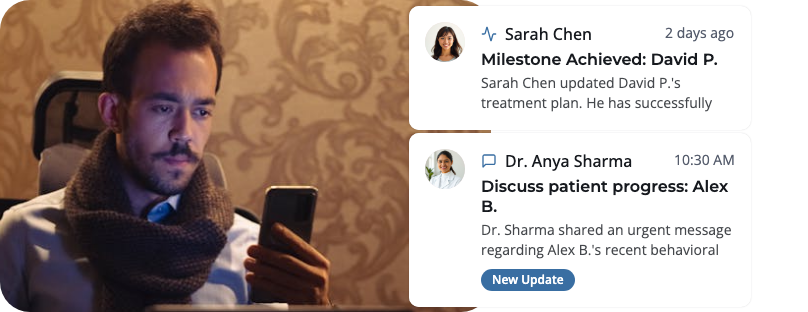
Connects behavioral health providers, case managers, and support teams in one platform.
Enables secure sharing of treatment updates, session notes, and progress milestones.
Facilitates real-time communication between care team members to prevent service gaps.
12%
higher appointment adherence when using technology-enabled care coordination
24%
improved depression symptom remission rates when using coordinated care models
85%
average therapy attendance rates using self-monitoring and adherence tracking tools
21%
reduction in relapse rates using early disengagement flagging with real-time tracking

Monitors therapy session attendance, medication adherence, and goal completion rates.
Flags early signs of disengagement for timely intervention by care coordinators.
Aggregates data into dashboards for compliance reporting and program optimization.
Jenny’s Story
Before you build more custom integrations or deploy disconnected point solutions, consider the HealthFeed advantage:



HealthFeed offers pre-built connectors for major EMRs, EHRs, CRMs, utilization management, and care management platforms (e.g., Cerner, Epic, ZeOmega). We also offer custom integrations and APIs, tailor built for your specific requirements and workflows.
We’re fully HIPAA‑compliant and built for CMS interoperability readiness. Additionally we adhere to GDPR, CPRA , and TX- RAMP guidelines. All data is encrypted in transit and at rest, with role‑based access controls, audit logging, and SOC‑2–certified infrastructure—so you can trust member and patient information stays private and secure.
Absolutely. HealthFeed’s white‑label member app and provider portal allow you to tailor UI/UX, messaging tone, and channel mix. Our AI‑driven personalization engine can be tuned with your clinical rules, reward programs, and specialty‑specific pathways so every outreach aligns with your brand and care protocols.
Most clients see measurable improvements within a few weeks: higher care‑gap closures, point boosts in CAHPS/HOS, and reduced avoidable utilization. Our real‑time analytics dashboards let you track metrics like outreach open rates, appointment adherence, and cost savings—so you can prove value from day one.
A typical rollout takes 6–8 weeks, including system integration, journey design workshops, and training. You’ll have a dedicated Customer Success Manager plus 24/7 support resources, regular strategy reviews, and access to our best‑practice playbooks to optimize engagement and continuously improve outcomes.