Comprehensive Diabetes Management: Tools and Strategies for Better Health
Discover HealthFeed's personalized diabetes management tools, from meal planning to CGM integration, for better health.
HealthFeed empowers care teams to engage members with precision. By unifying clinical data, automating care plans, and personalizing outreach, we help health plans close gaps, reduce costs, and improve outcomes—without adding complexity.


.png)
.png)
.png)

.png)


Managing care today goes beyond clinical data—it’s about engaging the whole person. Yet most health plans and care teams struggle with:
Closing care gaps isn’t just about clinical interventions. Members face everyday barriers that prevent them from accessing care and following treatment plans:
.svg)
Disparate systems create blind spots in member care.
.svg)
Outreach often fails to reach or resonate with the members who need it most.

.svg)
Addressing HEDIS, behavioral health, and SDOH gaps requires coordinated workflows.
.svg)
Generic communication limits outcomes and erodes trust.
HealthFeed gives care teams a centralized, intelligent platform to track, manage, and engage members—especially high-risk populations—across their entire health journey.
.png)
Unify structured and unstructured data from care management systems to create a real-time Member 360 view, including:
Medical history, allergies, conditions, medications
Risk scores and recent health events
Upcoming appointments and recent activity
Assigned care plans and open gaps
40%
Reduction in hospital readmission rates when using analytics and workflows
$3.1 Billion
Size of global healthcare data integration market by 2030
38%
lower no-show rate among patients receiving text reminders vs. no reminders
11x
more likely for high risk patients to miss their appointments without a second text reminder
.png)
Leverage AI to deliver tailored content and nudges through members’ preferred channels:
Text messages with care reminders or education
Email follow-ups on pending tasks
IVR calls for check-ins or follow-through
.png)
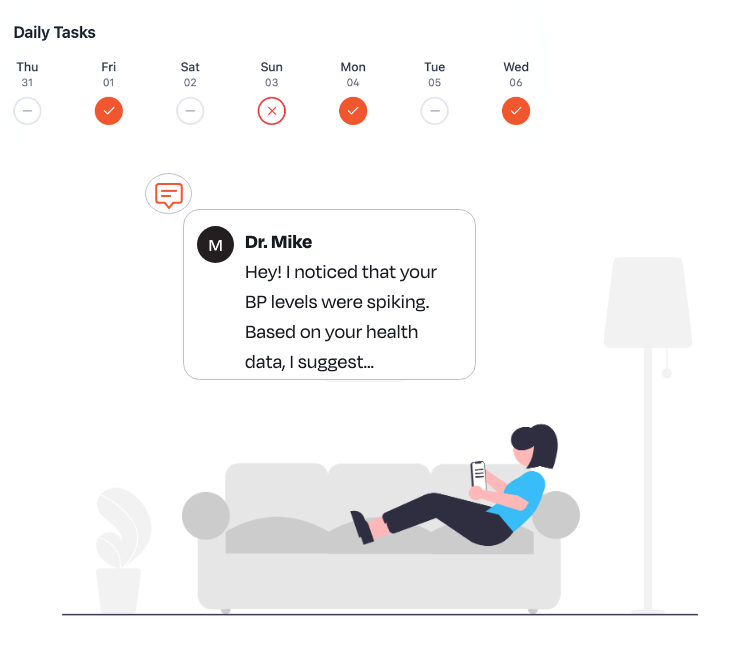
Streamline interventions across use cases—from post-discharge follow-ups to chronic care plans—with:
Prebuilt care plan templates
Task tracking with progress dashboards
Automatic nudges and reminders based on inactivity or risk triggers
43.5%
decrease in medication administration errors after implementing BCMA technology
$95 Billion
Size of global healthcare automation market by 2034
94%
accuracy in early disease detection by AI algorithms, surpassing radiologists
28%
reduction in revenue leakage by adopters of predictive analytics for health systems

Spot risks before they escalate and act faster with AI-driven insights.
Flags outliers and care gaps using machine learning
Surfaces risk-based alerts for timely intervention
Recommends next-best actions for care teams
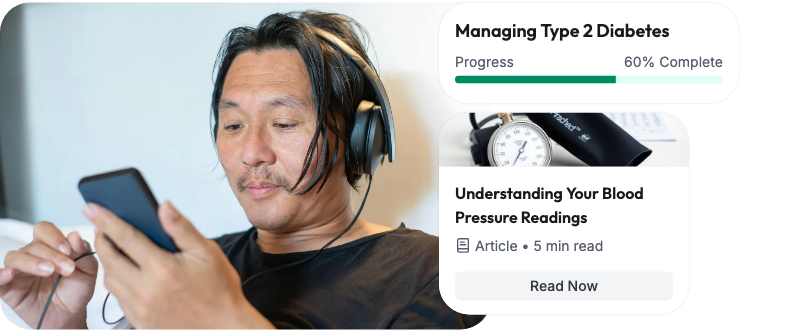
Deliver the right content to the right member—at the right time.
Assigns curated articles, videos, and behavior-change journeys
Supports education across chronic, behavioral, and lifestyle needs
Enables uploads of custom, plan-specific resources
95%
utilization of patient-portal educational resources in trials where usage was voluntary
1.67x
more likely for patient-portal users to attend scheduled appointments
Sally’s Story
.png)
.png)
.png)
Behind the scenes, HealthFeed tracks her engagement, progress, and open gaps—allowing her care team to adjust goals, assign new content, and keep her supported every step of the way.
Before you build more custom integrations or deploy disconnected point solutions, consider the HealthFeed advantage:



HealthFeed offers pre-built connectors for major EMRs, EHRs, CRMs, utilization management, and care management platforms (e.g., Cerner, Epic, ZeOmega). We also offer custom integrations and APIs, tailor built for your specific requirements and workflows.
We’re fully HIPAA‑compliant and built for CMS interoperability readiness. Additionally we adhere to GDPR, CPRA , and TX- RAMP guidelines. All data is encrypted in transit and at rest, with role‑based access controls, audit logging, and SOC‑2–certified infrastructure—so you can trust member and patient information stays private and secure.
Absolutely. HealthFeed’s white‑label member app and provider portal allow you to tailor UI/UX, messaging tone, and channel mix. Our AI‑driven personalization engine can be tuned with your clinical rules, reward programs, and specialty‑specific pathways so every outreach aligns with your brand and care protocols.
Most clients see measurable improvements within a few weeks: higher care‑gap closures, point boosts in CAHPS/HOS, and reduced avoidable utilization. Our real‑time analytics dashboards let you track metrics like outreach open rates, appointment adherence, and cost savings—so you can prove value from day one.
A typical rollout takes 6–8 weeks, including system integration, journey design workshops, and training. You’ll have a dedicated Customer Success Manager plus 24/7 support resources, regular strategy reviews, and access to our best‑practice playbooks to optimize engagement and continuously improve outcomes.