A Smarter CRM for Healthcare Teams
Unify data, close care gaps, and deliver personalized engagement at scale. HealthFeed makes population management proactive, connected, and efficient.
Request a Demo

.png)
.png)
.png)


















































Everything You Need to Power Smarter Care
Streamline care with integrated data, predictive insights, automated outreach, and connected team workflows, all in one intelligent CRM.

Integrated Member 360 View
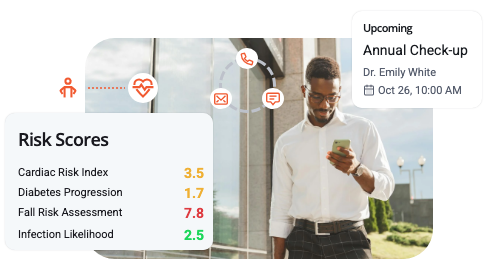
Predictive Risk & Care Insights
Intelligent Multi‑Channel Outreach
Seamless Care Coordination Tools
All Your Healthfeed Features, On The Go
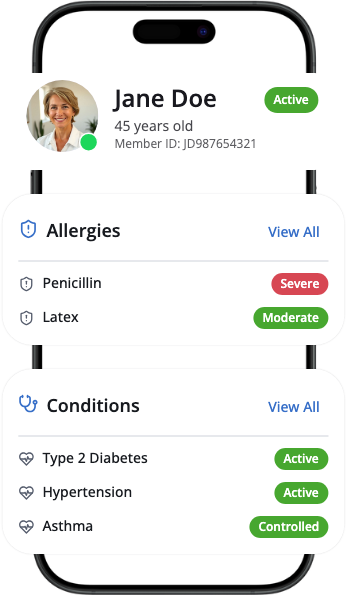
Integrated Member 360 View
Bring all data into one place with a real‑time member profile, giving care teams full visibility into history, risks, and care gaps to streamline decision‑making.
Unified medical, claims, lab, and CRM data
Complete view of allergies, conditions, and medicines
NCQA‑compliant quality gap tracking
Social determinants mapped to member care
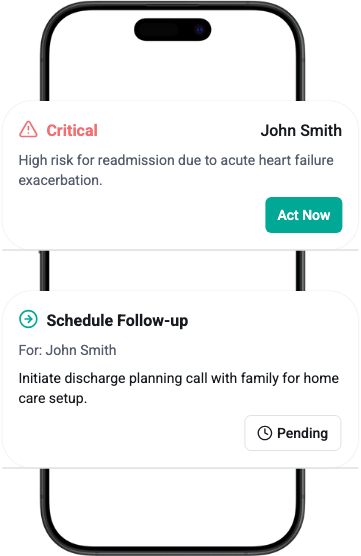
Predictive Risk and Care Insights
Use intelligent predictive analytics to anticipate health risks, identify rising‑risk members, and guide teams with recommended next best actions for timely interventions.
Intelligent insights flag care gaps and outliers early
Risk‑based alerts for urgent needs
Predictive models for engagement and adherence
Proactive support for SDOH challenges
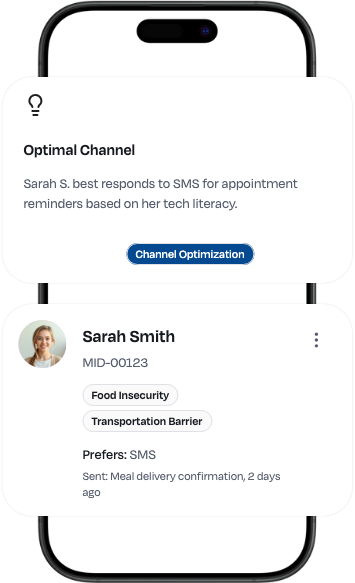
Intelligent Multi‑Channel Outreach
Engage members through automated, personalized communication delivered via preferred channels, improving adherence, response rates, and overall member trust.
SMS, email, IVR, chat, and mail campaigns
Reminders, confirmations, and rescheduling prompts
Language and culture‑adapted education
Outreach triggered by inactivity or missed care
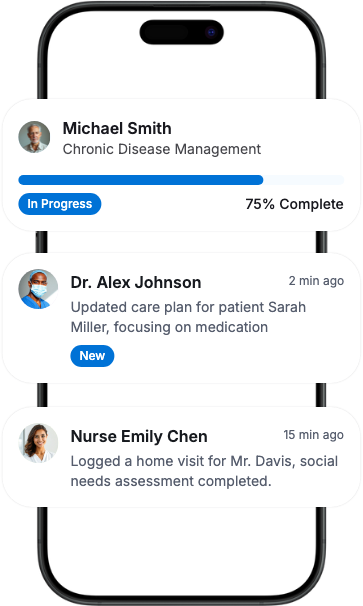
Seamless Care Coordination Tools
Empower care teams with shared tools that connect providers, streamline workflows, and deliver coordinated care across clinical, behavioral, and social needs.
Shared platform for providers and case managers
Secure, real‑time updates and communication
Pre‑built care plan templates and workflows
Task automation to close gaps quickly
Benefits that Empower You
Reduced No‑Shows
Timely SMS, email, or IVR reminders ensure members keep appointments, while automated follow‑ups quickly re‑engage missed visits.
Faster Gap Closures
Predictive alerts and task automation flag open quality gaps and route them to the right care team member for quicker resolution.
Smarter Member Outreach
AI‑driven messaging adapts to culture, language, and literacy levels, improving member response rates and program participation.
Connected Care Teams
Shared dashboards and secure communication tools keep providers, case managers, and behavioral health specialists aligned in real time.