Comprehensive Diabetes Management: Tools and Strategies for Better Health
Discover HealthFeed's personalized diabetes management tools, from meal planning to CGM integration, for better health.
HealthFeed helps health plans and care teams manage entire populations with precision. From identifying rising-risk members to activating personalized care plans, our AI-powered platform reduces costs, boosts engagement, and improves health outcomes—at scale.


.png)
.png)
.png)



Managing population health sounds simple—until you try it. Most health plans struggle with:
Closing care gaps isn’t just about clinical interventions. Members face everyday barriers that prevent them from accessing care and following treatment plans:
.svg)
Disparate data sources and poor integration prevent a unified member health view, hindering care coordination and informed decision-making across providers and plans.
.svg)
Slow or insufficient data analysis delays recognizing at-risk members, reducing the chance for early intervention and timely care that may prevent costly health complications.
.svg)
Care teams working independently lack shared information, causing miscommunication, care gaps, and delayed action, ultimately impacting member outcomes and satisfaction.

.svg)
Members may not actively participate in their care, reducing treatment adherence and making it hard for health plans to influence positive health behaviors or outcomes.
.svg)
Insufficient transparency in tracking care outcomes makes it challenging to measure impact, demonstrate ROI, and refine population health management strategies.
.svg)
Generic communication limits outcomes and erodes trust.

Bring all your data together for a real-time, unified perspective.
Connects EMRs, EHRs, CRMs, and claims via APIs or prebuilt connectors
Offers a 360° member profile including history, gaps, goals, and activity
Enables targeted segmentation by condition, risk score, or care stage
63%
reduction in hospital readmission rates when using integrated population data frameworks
76%
improvement in Chronic disease management metrics with unified, real-time patient data integration.
17%
improvement in protocol compliance using AI-driven predictive analytics
3:1
ratio of healthcare cost savings to spending on preventive predictive analytics
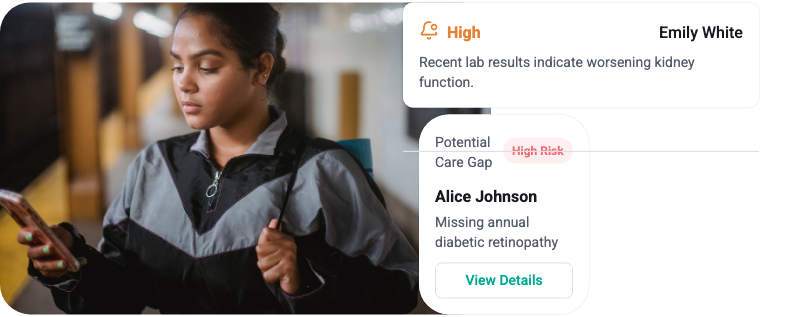
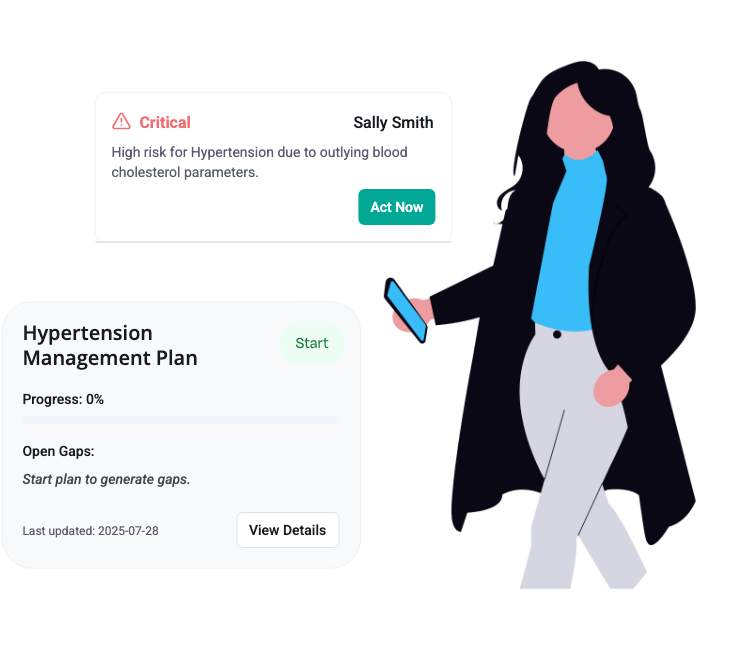
Act before risks become readmissions.
Uses AI to surface rising-risk members and potential health events
Flags care gaps and outliers in real time
Recommends next-best actions for proactive care
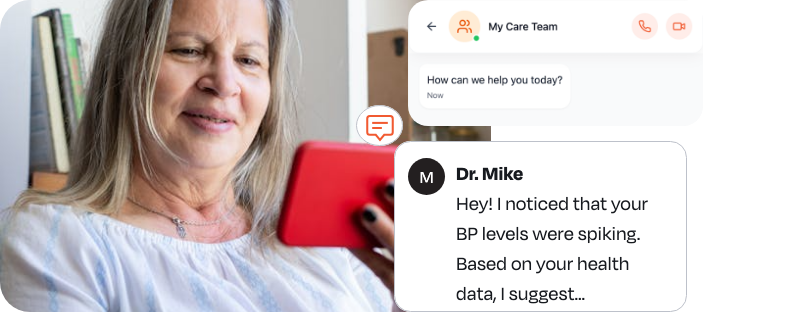
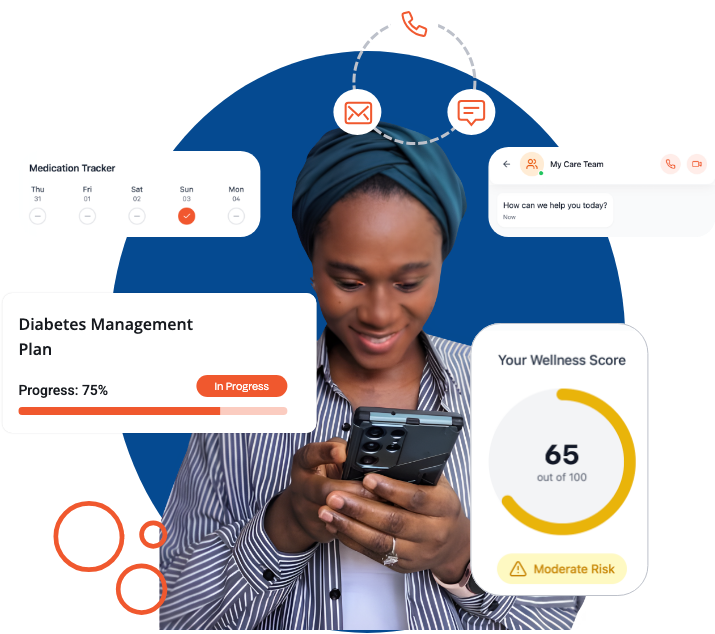
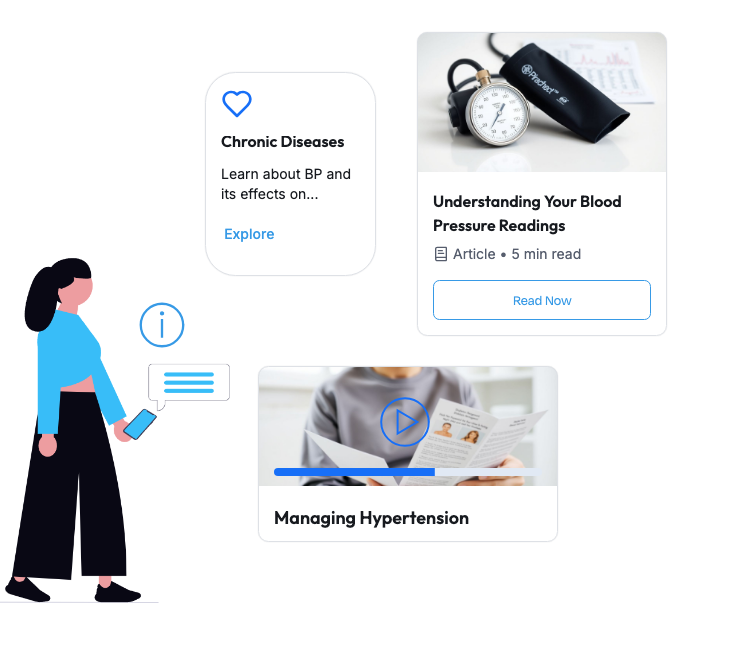
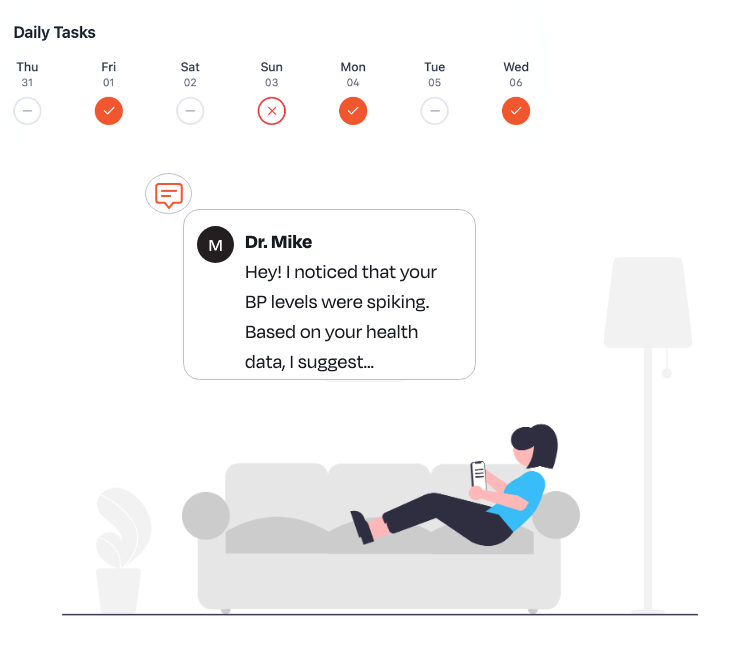
Reach members where they are—with messages that resonate.
Sends tailored nudges via SMS, email, or IVR
Triggers outreach based on inactivity, non-adherence, or risk flags
Keeps communication timely, human, and actionable
3x
higher patient engagement rate when using automated personalized outreach solutions
94%
appointment booking success rate when using automated personalized outreach tools.
18%
improvement in patient attainment of disease control goals having a personalized care plan
22%
improvement in health-related quality-of-life scores after implementing care plans,

Deliver the right intervention, at the right time.
Assigns condition-specific plans for chronic and preventive care
Tracks member progress on tasks, goals, and content engagement
Allows care managers to adapt plans in real time

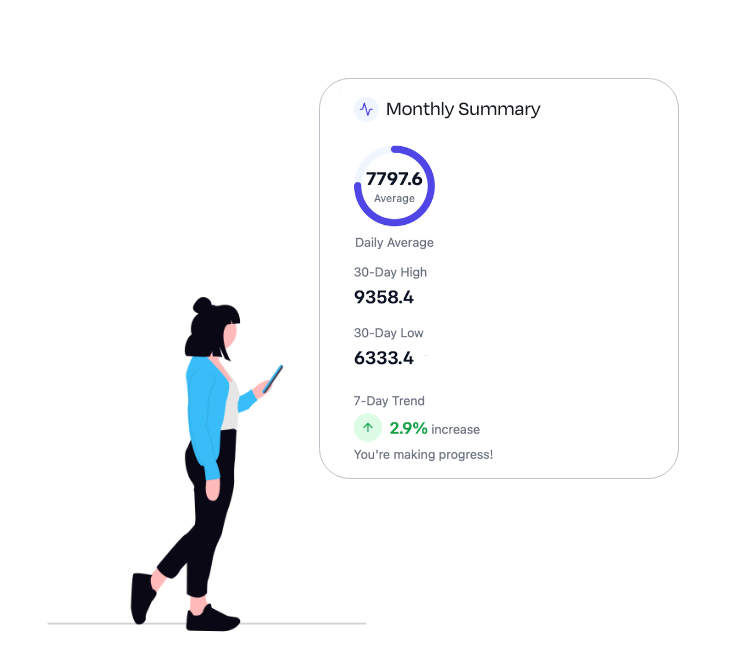
Know what’s working—and what’s not.
Dashboards track engagement, adherence, and outcome improvements
Visualize population trends and program ROI
Export insights to inform strategy and reporting
3.2x
average ROI from engagement initiatives with real-time impact measurement.
6 Billion+
people's progress tracked by WHO's outcome measurement system globally
48%
Reduction in healthcare data breaches in the US since the onset of HIPAA and related initiatives
80%
fewer breach-related incidents in compliant organizations
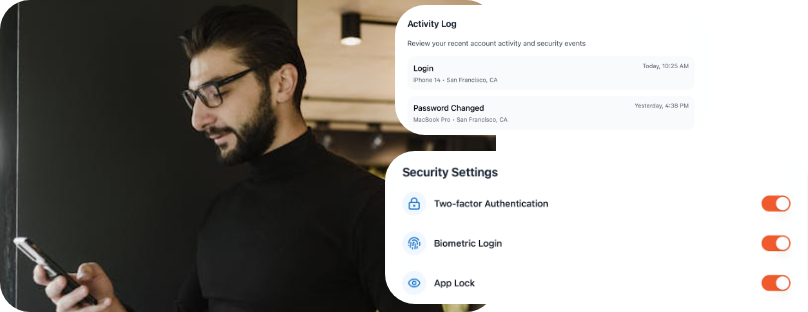
Built for trust in every workflow.
HIPAA, GDPR, CPRA-compliant with full encryption
Role-based access controls for different user levels
Audit trails for outreach, data updates, and task changes
Sally’s Story

Before you build more custom integrations or deploy disconnected point solutions, consider the HealthFeed advantage:



HealthFeed offers pre-built connectors for major EMRs, EHRs, CRMs, utilization management, and care management platforms (e.g., Cerner, Epic, ZeOmega). We also offer custom integrations and APIs, tailor built for your specific requirements and workflows.
We’re fully HIPAA‑compliant and built for CMS interoperability readiness. Additionally we adhere to GDPR, CPRA , and TX- RAMP guidelines. All data is encrypted in transit and at rest, with role‑based access controls, audit logging, and SOC‑2–certified infrastructure—so you can trust member and patient information stays private and secure.
Absolutely. HealthFeed’s white‑label member app and provider portal allow you to tailor UI/UX, messaging tone, and channel mix. Our AI‑driven personalization engine can be tuned with your clinical rules, reward programs, and specialty‑specific pathways so every outreach aligns with your brand and care protocols.
Most clients see measurable improvements within a few weeks: higher care‑gap closures, point boosts in CAHPS/HOS, and reduced avoidable utilization. Our real‑time analytics dashboards let you track metrics like outreach open rates, appointment adherence, and cost savings—so you can prove value from day one.
A typical rollout takes 6–8 weeks, including system integration, journey design workshops, and training. You’ll have a dedicated Customer Success Manager plus 24/7 support resources, regular strategy reviews, and access to our best‑practice playbooks to optimize engagement and continuously improve outcomes.