Healthcare Plans
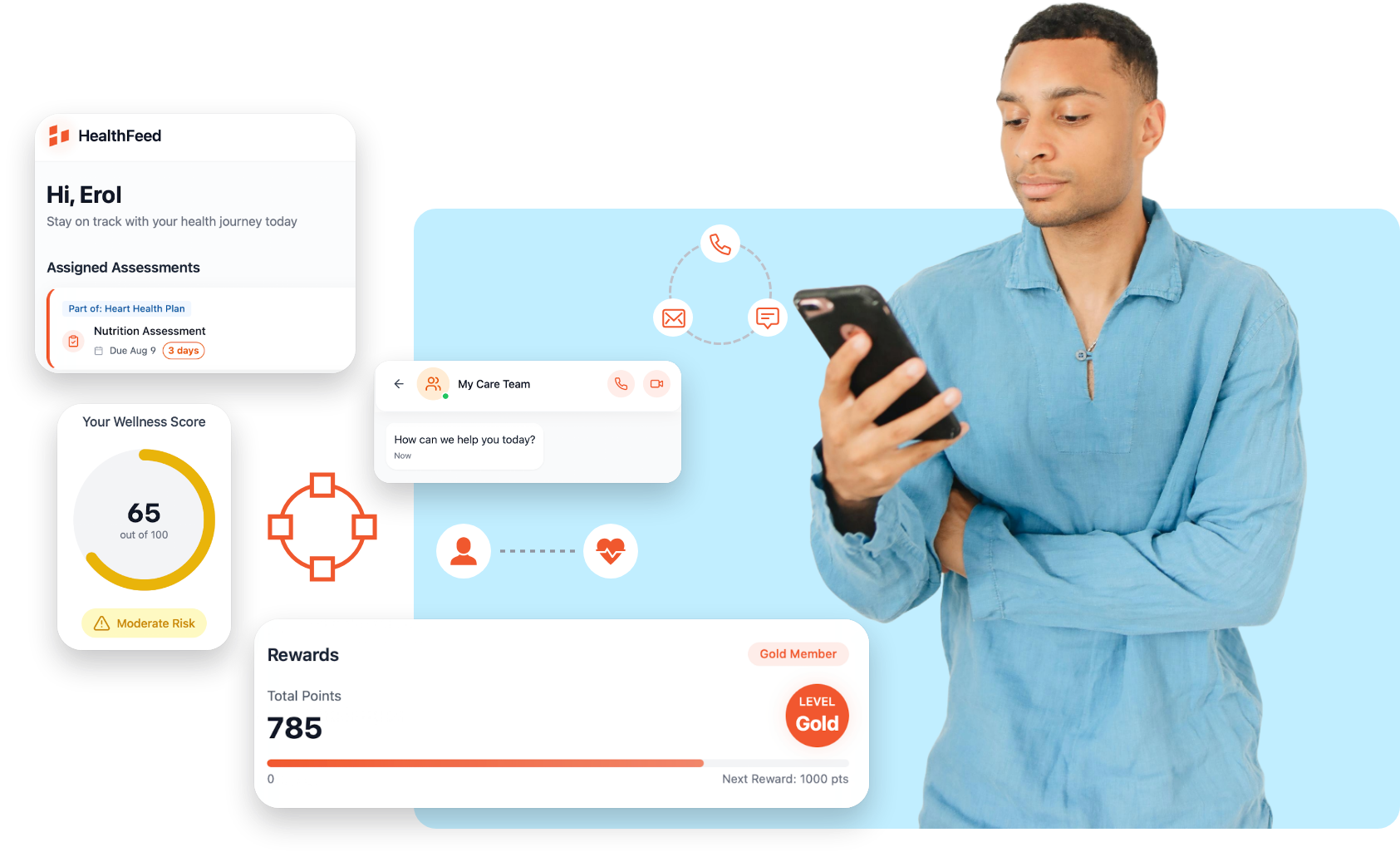
HealthFeed equips health plans with AI-powered tools to unify data, engage members, close gaps, and drive measurable outcomes, reducing costs while improving satisfaction and compliance.
of Medicaid enrollees face at least one social risk factor, but most plans still use paper-based assessments
potential annual savings in the U.S. by shifting to digitally-enabled care coordination
of health plans say automated outreach improves care gap closure and reduces operational costs
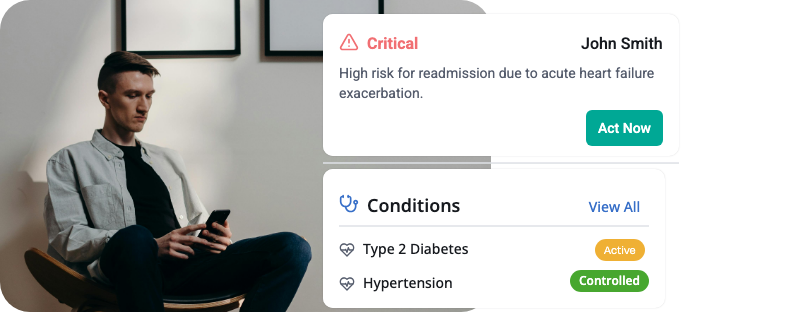
HealthFeed integrates data for real-time risk identification and automated outreach, optimizing chronic and preventive care.
Connects EMRs, claims, and more for a 360° member view.
Uses AI to flag rising risks and recommend actions.
Segments populations by condition or risk for targeted plans.
63%
reduction in hospital readmission rates when using integrated population data frameworks
76%
improvement in Chronic disease management metrics with unified, real-time patient data integration.
40%
reduction in readmissions using analytics and workflows.
38%
lower no-show rates with text reminders.
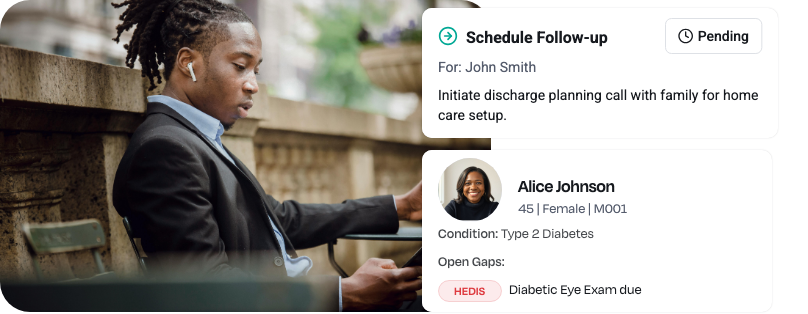
HealthFeed unifies clinical data and automates plans to engage high-risk members and reduce administrative burden.
Creates real-time Member 360 views with history and gaps.
Delivers tailored nudges via preferred channels like SMS.
Automates tasks and reminders for post-discharge follow-ups.

HealthFeed digitizes screenings and connects members to resources, turning SDoH insights into actionable interventions.
Integrates screening tools like PRAPARE with care workflows.
Automates referrals and reminders for community support.
Tracks social risks alongside clinical data for holistic views.
85%
of enrollees with social risks, mitigated by digital assessments.
40%
readmission drop with barrier-focused analytics.
72%
of plans see gap closure gains from automation.
11x
higher appointment risks without reminders.
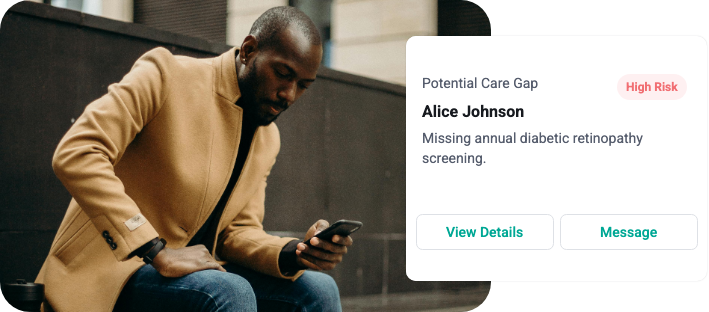
HealthFeed ingests quality data to identify gaps, automate outreach, and track compliance for improved Star Ratings.
Maps gaps to members with NCQA-compliant tracking.
Prioritizes urgent measures and escalates outreach.
Provides dashboards for real-time performance monitoring.

HealthFeed supports screenings, reminders, and team collaboration to reduce no-shows and improve behavioral outcomes.
Automates appointment management and follow-ups.
Delivers personalized, stigma-reducing content.
Enables secure sharing across providers and managers.
38%
no-show reduction with reminders.
94%
accuracy in early detection via AI.
HealthFeed offers pre-built connectors for major EMRs, EHRs, CRMs, utilization management, and care management platforms (e.g., Cerner, Epic, ZeOmega). We also offer custom integrations and APIs, tailor built for your specific requirements and workflows.
We’re fully HIPAA‑compliant and built for CMS interoperability readiness. Additionally we adhere to GDPR, CPRA , and TX- RAMP guidelines. All data is encrypted in transit and at rest, with role‑based access controls, audit logging, and SOC‑2–certified infrastructure—so you can trust member and patient information stays private and secure.
Absolutely. HealthFeed’s white‑label member app and provider portal allow you to tailor UI/UX, messaging tone, and channel mix. Our AI‑driven personalization engine can be tuned with your clinical rules, reward programs, and specialty‑specific pathways so every outreach aligns with your brand and care protocols.
Most clients see measurable improvements within a few weeks: higher care‑gap closures, point boosts in CAHPS/HOS, and reduced avoidable utilization. Our real‑time analytics dashboards let you track metrics like outreach open rates, appointment adherence, and cost savings—so you can prove value from day one.
A typical rollout takes 6–8 weeks, including system integration, journey design workshops, and training. You’ll have a dedicated Customer Success Manager plus 24/7 support resources, regular strategy reviews, and access to our best‑practice playbooks to optimize engagement and continuously improve outcomes.